 New research reveals impaired oxygen absorption and mitochondrial dysfunction in muscle cells may explain why exercise makes long COVID patients feel worse. Depositphotos –
New research reveals impaired oxygen absorption and mitochondrial dysfunction in muscle cells may explain why exercise makes long COVID patients feel worse. Depositphotos –
In most instances of rehabilitation, exercise is a beneficial thing. And when a patient is struggling with exercise there are usually obvious physiological explanations. Maybe the heart or lungs are not functioning well, or maybe an extended period of illness led to a kind of physical deconditioning where the body has generally weakened.
However, in many long COVID cases there are no obvious signs to explain these exercise limitations. Many patients have been subjected to a barrage of conventional tests only to be told they seem to be completely fine. But several new studies are starting to figure out the mystery behind long COVID PEM. And although the findings don’t immediately point to solutions, they affirm these long COVID-related exercise intolerances do have physiological foundations.
The most traditional test of a patient’s functional physical capacity is called a cardiopulmonary exercise test (CPET). A patient is put on an exercise bike while doctors monitor heart rate, oxygen saturation and electrocardiogram data.
For many long COVID patients CPET investigations return unusually normal results. Despite their obvious exercise limitations such as shortness of breath, these patients often show normal oxygen levels and healthy heart function.
A new study from a team of researchers at Yale University recruited a cohort of long COVID patients for a novel CPET experiment. The test is known as iCPET (invasive cardiopulmonary exercise test) and it is not as simple as a regular CPET. Alongside the regular CPET measures, patients undergoing this test have two pressure-sensing catheters inserted into arteries. This allows for extra insight into the effect of exercise on muscles and blood vessels.
The results were striking, revealing no notable problems with the way the heart or lungs were functioning but distinct abnormalities in the way the body’s tissues were taking up oxygen. The dysfunction was labeled as impaired peak systemic oxygen extraction (pEO2).
“We found that despite the fact that the heart was pumping oxygenated blood that the lungs were providing adequate amounts of oxygen for, the extraction of oxygen by the body’s tissues was compromised in patients who had symptoms of exercise intolerance after COVID,” explained lead author on the study, Peter Kahn.
Exactly why or how this was happening, however, could only be hypothesized, with the researchers flagging several possible explanations for this unusual phenomenon.
“Impaired pEO2 can be attributable to failure of non-exercising vascular beds to vasoconstrict or direct intramuscular blood flow appropriately, or capillary-to-mitochondrial diffusion inadequacy,” the authors speculate in the study.
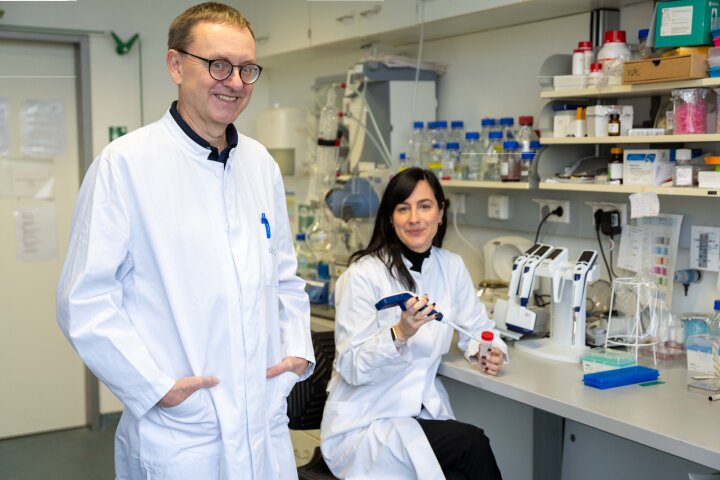
A recently published study in Nature Communications, from a team of scientists in Amsterdam, offers intriguing clues to what may be going on. And the answer seems to have something to do with mitochondria – the tiny powerplants energizing individual cells.
This extraordinarily unique experiment gathered a cohort of long COVID patients and a healthy control group. The volunteers completed a strenuous cycling test supplying blood and muscle tissue samples one week before and one day after the test.
Rob Wüst, a co-author on the study, said metabolic impairments and signs of significant muscle damage were detected in the long COVID patients after strenuous exercise. Perhaps most significantly, the findings revealed strenuous exercise actually triggered mitochondrial dysfunction in muscle cells, and this may explain why long COVID patients feel worse the day after physical exertion.
“We saw various abnormalities in the muscle tissue of the patients,” Wüst explains. “At the cellular level, we saw that the mitochondria of the muscle, also known as the energy factories of the cell, function less well and that they produce less energy.”
While these two studies affirm long-COVID-related exercise intolerance and post-exertional malaise certainly have physiological foundations, there are still lots of unanswered questions. Mitochondrial dysfunction has previously been hypothesized as a potential explanation for some long COVID symptoms, but exactly how a SARS-CoV-2 infection causes this is still a mystery.
Viral persistence has been floated as one explanation but Wüst and colleagues somewhat ruled that hypothesis out by finding similar levels of SARS-CoV-2 fragments in skeletal muscles of both long COVID patients and control subjects. When pushed to speculate, Wüst suggests the big mystery is how this virus is altering mitochondrial function in muscle cells.
“I personally don’t think that the mito dysfunction is a result of something else going wrong,” Wüst says to New Atlas. “The reason for this is that exercise is always regarded beneficial for mito function, and this is not the case for [long COVID] patients. Obviously muscle damage and the resulting infiltration of immune cells can reduce mito function too, or an unknown factor X is causing mito dysfunction.”
A treatment for long COVID exercise intolerance may be a little ways off but these findings can at least assuage patients who often are made to feel their symptoms are all in their head after standard tests return normal results. Brent Appelman, a co-author on the Amsterdam study, says long COVID patients should be cautious to not push physical exertion beyond their limits. It is now increasingly clear that excessive exertion is damaging and we are starting to understand why.
“In concrete terms, we advise these patients to guard their physical limits and not to exceed them,” Appelman says. “Think of light exertion that does not lead to worsening of the complaints. Walking is good, or riding an electric bike, to maintain some physical condition. Keep in mind that every patient has a different limit.”
The Yale study was published in the journal ERJ Open Research and the Amsterdam study was published in Nature Communications.
–