 Targeting progesterone receptors in the brain may be a route to migraine relief for some people. We Are/DigitalVision via Getty Images
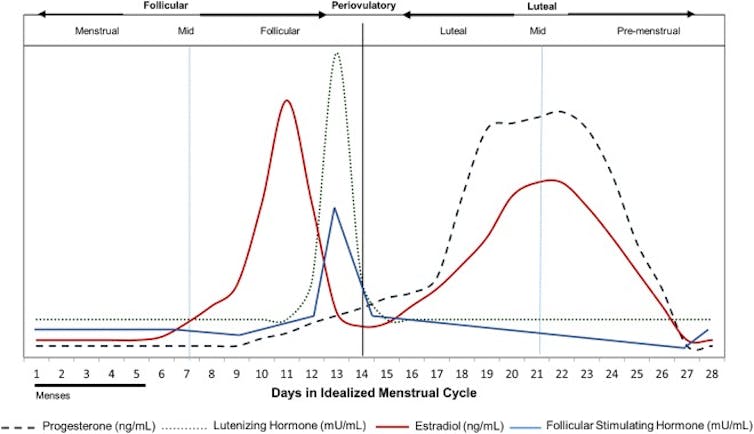
Targeting progesterone receptors in the brain may be a route to migraine relief for some people. We Are/DigitalVision via Getty ImagesMigraines often occur around the menstrual cycle, during which reproductive hormones such as progesterone and estrogen rise and fall. The levels of both these hormones are low during the perimenstrual period.
Some patients experience headaches exclusively during menstruation, called menstrual migraines. These migraines tend to be more severe and more challenging to treat than episodes occurring before or after menstruation. Repeated migraine episodes increase the risk of chronic migraines. Uncontrolled migraines could also increase the risk of headaches from the overuse of medication.
–
We are researchers who study how progesterone regulates neuronal function in health and disease. Our research over the past several years has focused on understanding how this hormone and its receptors affect the brain. In our recently published research in mice, we found that progesterone may make people who menstruate more susceptible to migraines.
Progesterone and pain sensitivity
First, we determined whether pain sensitivity in female mice changes during their reproductive cycle. Female mice experience cyclic hormonal changes during what are called estrous cycles that last for four to five days.
To do this, we applied thin wires of increasing weight to the mice’s hind paws to determine their touch sensitivity. The mice signaled discomfort by withdrawing their paw. We found that pain sensitivity was higher in mice at the end of the cycle when reproductive hormone levels are low compared to mice in mid-cycle when reproductive hormone levels are high.
Next, we tested whether progesterone increased pain sensitivity. We removed the mice’s ovaries to eliminate internally-driven hormonal changes. Since an estrogen surge precedes progesterone release during female reproductive cycles, we administered estrogen followed by progesterone or saline. We found that progesterone-treated animals had increased touch sensitivity, but not the saline-treated animals.
Progesterone exerts its effects in part by stimulating proteins called progesterone receptors that are located in the brain, slowly modulating the expression of different genes. Progesterone can also quickly alter how neurons function when it breaks down into a molecule called allopregnanolone. Our studies suggest progesterone receptors may play a role in the slow-emerging, pain-promoting effect of progesterone.
–
After finding progesterone receptors in neurons that form a part of migraine pain pathways in the brain, we next wanted to know whether these receptors regulate migraine susceptibility. In mice without progesterone receptors in their brains, progesterone did not reduce their pain threshold. In contrast, activating progesterone receptors using a drug that specifically targets those receptors increased pain susceptibility. Progesterone regulated sensitivity to mechanical and cold stimuli but not sensitivity to heat and light stimuli.
Finally, we used nitroglycerin to mimic migraines. Nitroglycerin produces symptoms similar to those seen in migraine patients, and many of the drugs used to treat migraines also resolve these symptoms in animals. When we stimulated mice’s progesterone receptors, migraine susceptibility increased. In contrast, mice lacking these receptors were resistant to nitroglycerin-induced pain.
Potential targets for migraine treatment
Our study identifies progesterone receptors in the brain as one reason women are susceptible to migraines. Cyclical changes in progesterone levels during the menstrual cycle activate the receptor, which can precipitate migraines.
This also means the progesterone receptor is a possible drug target for preventing or treating migraines. As our team continues to study how progesterone receptors increase pain sensitivity, we hope to uncover new ways to treat migraine headaches.
–
- Neuroscience
- Hormones
- Neurology
- Headaches
- Pain
- Migraine
- Menstruation
- Sex differences
- Progesterone
- Sex hormones
- Menstrual cycle
- New research
- reproductive hormones
- STEEHM new research
–
Jaideep Kapur receives funding from the National Institute of Neurological Disorders and Stroke.
Partners

University of Virginia provides funding as a member of The Conversation US.
View all partners
Republish our articles for free, online or in print, under a Creative Commons license.
–
Want to write?
Write an article and join a growing community of more than 188,100 academics and researchers from 5,012 institutions.












