 A new gene therapy lowered two heart disease-related lipids in a human clinical trial. Depositphotos –
A new gene therapy lowered two heart disease-related lipids in a human clinical trial. Depositphotos –
The angiopoietin-like protein 3 (ANGPTL3) gene is a liver fat brake, telling the body to slow the clearance of fats such as low-density lipoprotein (LDL, the “bad”) cholesterol and triglycerides from the blood. Some people are born with a mutation that turns this brake off leaving these lipids unusually low.
Scientists from the Victorian Heart Hospital and the Victorian Heart Institute, in partnership with Monash University, have conducted the first-in-human clinical trial of a breakthrough gene therapy that mimics this condition in people with hard-to-treat lipid disorders.
“The best way to treat heart disease, the leading cause of death for both men and women globally, is to prevent it,” said the trial’s lead investigator, Professor Stephen Nicholls, Director of the Victorian Heart Hospital and the Victorian Heart Institute. “Gene-editing technology is a new frontier of medical treatment, and it’s incredibly exciting for Victorians and Australians that we are leading such an important trial.”
The ANGPTL3 gene provides instructions for making the protein angiopoietin-like protein 3, which is produced almost entirely in the liver and released into the bloodstream. In the blood, a key enzyme called lipoprotein lipase (LPL) sits on blood vessel walls and breaks down triglycerides so tissues can use or store the fat. ANGPTL3 acts by inhibiting this enzyme. It also inhibits another enzyme, endothelial lipase, which helps remodel high-density lipoprotein (HDL or “good”) cholesterol. So, when ANGPTL3 is active, fat and cholesterol are cleared more slowly, blood levels tend to be higher, and triglycerides and LDL cholesterol go up.
For people born with loss-of-function mutations in ANGPTL3, the gene doesn’t work properly or at all. These people have unusually low levels of triglycerides, LDL and HDL, a condition called familial combined hypolipidemia. They also appear to have a lower risk of cardiovascular disease. So, turning down or off ANGPTL3 is protective from a heart-disease perspective, at least in terms of lipids. The compound CTX310, a new CRISPR-Cas 9 gene-editing therapy, is essentially designed to copy this naturally protective genetic state in people whose lipids remain stubbornly high despite standard treatments.
Fifteen adults participated in the trial; all had elevated lipids despite treatment. Each person got a single intravenous (IV) infusion of CTX310 at different doses, from 0.1 to 0.8 mg/kg. Within about two weeks of the infusion, participants’ LDL and triglycerides started dropping.
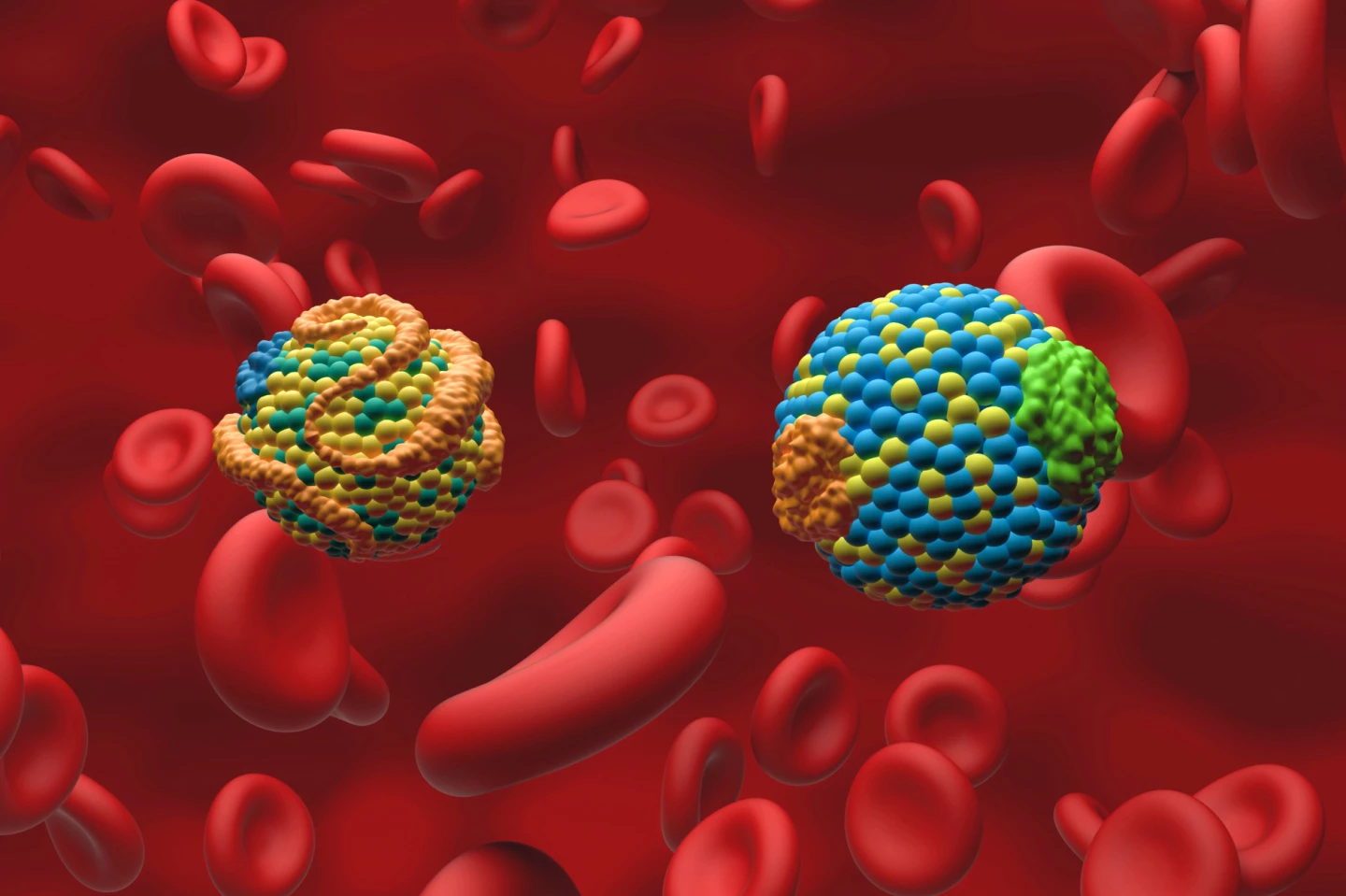
After 60 days, the highest dose produced a drop in LDL of about 50% and about a 55% drop in triglycerides. Across the full Phase 1 trial, later data from the full cohort showed peak reductions of around 80% or more in both LDL and triglycerides at higher doses.
Effects lasted at least 60 days, which is basically the length of formal follow-up for this early dataset. Reported side effects were mild and short-lived and included things like flu-like symptoms. No serious safety concerns were raised thus far, though participants will be followed for 15 years, which is standard for in vivo gene editing.
“The Phase 1 clinical trial of CTX310 shows the treatment is both possible and safe for people,” Nicholls said. “If confirmed in future phases and larger trials, this one-time treatment has the potential to help save millions of lives worldwide from heart disease each year.”
This clinical trial is a big deal for a few reasons. The first is that it pushes CRISPR – which has so far been used mainly for rare, severe genetic diseases such as sickle cell anemia – into mass-prevalence territory by treating cardiovascular risk factors like high LDL and triglycerides. Secondly, it is a one-and-done treatment that directly tackles the huge real-world problem of people not sticking to statins (lipid-lowering medications) or injections long-term. Third, most current drugs are better at lowering LDL cholesterol or triglycerides, not both together.
Of course, as with any study, there are caveats. It was a very small, early trial that was designed to look at safety and biology, not heart-attack/stroke outcomes. We’re years away from knowing if this actually reduces events and by how much. Additionally, the follow-up, at 60 days, was short. The true lifetime durability is unknown. There’s also the irreversibility aspect of the treatment; once ANGPTL3 is switched off, it can’t be switched back on. Finally, there’s the accessibility angle: who gets this treatment? If pricing follows other gene therapies, it could easily land in six-figure territory per treatment at launch. That might still be cost-effective in extreme-risk patients, but it’s a huge health-economics and equity conversation.
Nevertheless, if the effects are reproduced in larger, longer trials, CTX310 has great potential.
“The possibility of a single-course treatment with lasting effects could be a major step in how we prevent heart disease,” said Nicholls. “It makes treatment …[for the balance of this very important article please visit: https://newatlas.com/medical-tech/gene-therapy-ctx310-ldl-cholesterol-triglycerides/]
–
Source: Monash University
–