Researchers have been able to accurately diagnose autism in children using AI to screen retinal photographs. Depositphotos
Researchers have been able to accurately diagnose autism in children using AI to screen retinal photographs. Depositphotos
–
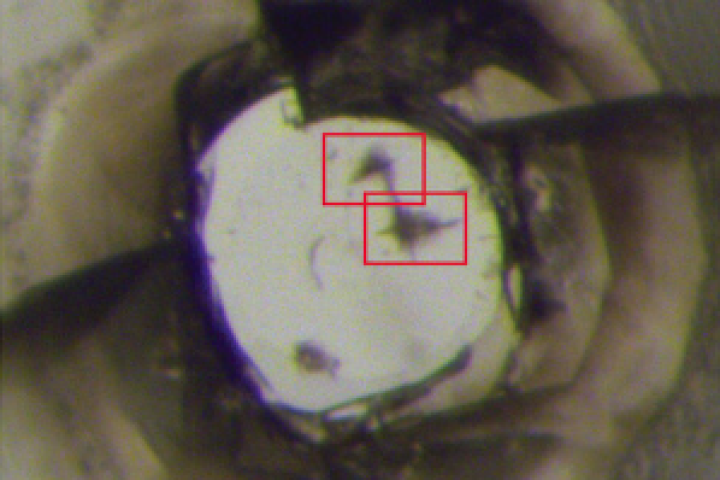
At the back of the eye, the retina and the optic nerve connect at the optic disc. An extension of the central nervous system, the structure is a window into the brain and researchers have started capitalizing on their ability to easily and non-invasively access this body part to obtain important brain-related information.
Recently, UK researchers created a non-invasive means of rapidly diagnosing concussion by shining an eye-safe laser onto the retina. Now, researchers from Yonsei University College of Medicine in South Korea have developed a method of diagnosing autism spectrum disorder (ASD) and symptom severity in children using retinal images screened by an AI algorithm.
The researchers recruited 958 participants with a mean age of 7.8 years and photographed their retinas, resulting in a total of 1,890 images. Half of the participants had been diagnosed with ASD, and half were age- and sex-matched controls. ASD symptom severity was assessed using Autism Diagnostic Observation Schedule – Second Edition (ADOS-2) calibrated severity scores and Social Responsiveness Scale – Second Edition (SRS-2) scores.
A convolutional neural network, a deep learning algorithm, was trained using 85% of the retinal images and symptom severity test scores to construct models to screen for ASD and ASD symptom severity. The remaining 15% of images were retained for testing.
For ASD screening on the test set of images, the AI could pick out the children with an ASD diagnosis with a mean area under the receiver operating characteristic (AUROC) curve of 1.00. AUROC ranges in value from 0 to 1. A model whose predictions are 100% wrong has an AUROC of 0.0; one whose predictions are 100% correct has an AUROC of 1.0, indicating that the AI’s predictions in the current study were 100% correct. There was no notable decrease in the mean AUROC, even when 95% of the least important areas of the image – those not including the optic disc – were removed.
“Our models had promising performance in differentiating between ASD and TD [children with typical development] using retinal photographs, implying that retinal alterations in ASD may have potential value as biomarkers,” said the researchers. “Interestingly, these models retained a mean AUROC of 1.00 using only 10% of the image containing the optic disc, indicating that this area is crucial for distinguishing ASD from TD.”
The mean AUROC value for symptom severity was 0.74, where an AUROC of 0.7 to 0.8 is considered ‘acceptable’ and 0.8 to 0.9 is ‘excellent’.
“Our findings suggest that retinal photographs may provide additional information regarding symptom severity,” the researchers said. “We observed that feasible classification was achievable only for ADOS-2 scores and not for SRS-2 scores. This may be because the ADOS-2 is conducted by a trained professional with ample time for assessment, whereas the SRS-2 is typically completed by a caregiver in a few dozen minutes; thus, the former would reflect one’s severity status more accurately than the latter.”
Study participants were as young as four. Based on their findings, the researchers say that their AI-based model could be used as an objective screening tool from that age onwards. Because the newborn retina continues to grow until the age of four, further research is needed to ascertain whether the tool would be accurate for participants younger than that.
“Although future studies are required to establish generalizability, our study represents a notable step toward developing objective screening tools for ASD, which may help address urgent issues such as the inaccessibility of specialized child psychiatry assessments due to limited resources,” said the researchers.
The study was published in the journal JAMA Network Open.
Source: Yonsei University College of Medicine via Scimex
–