–
Tens of thousands of ordinary greenbottle flies are swarming inside 30 boxes in a cleanroom at an unassuming building in a south Wales business park, where passersby would not suspect that insect eggs are regularly collected to breed larvae for “maggot therapy” in the NHS (National Health Service).
Hundreds of UK health service hospitals as well as clinics in Germany are using maggots to clean chronic wounds such as diabetic leg ulcers and speed up the healing process – reviving a centuries-old tradition practiced by Maya tribes in Central America and Indigenous Australians.
During the first world war, US doctor William Baer realized wounds with maggots in them healed much faster than those without. He started growing larvae on a hospital windowsill to treat patients with osteomyelitis, a bone inflammation. By the end of the 1930s, 300 hospitals in the US and Canada were using maggots, but their use declined with the arrival of penicillin and other antibiotics, only to be rediscovered in the 1990s amid growing antibiotic resistance.
There has been a revival of the therapy worldwide, which has been available as a prescribed NHS treatment since 2004, when it also received regulatory approval in the US. Clinical-grade larvae are reared in the US, Australia, China, Turkey and across Africa, for example in Nigeria.
“These are not the maggots that you find crawling in sewage or in your dustbins, these are clinically reared,” says Prof Yamni Nigam at Swansea University, an expert on the science and therapeutic use of maggots.
BioMonde, based in Bridgend, south Wales, is among those at the forefront of larval therapy, where greenbottle fly larvae are grown in the lab, disinfected, and put into finely woven net pouches about the size of a teabag that are then placed on patients’ wounds for four days. The maggots work their magic through the material and the bags are removed before they turn into flies.
–
“People are shocked at how effective it is,” says Vicky Phillips, a former tissue viability nurse at Hampshire Hospitals NHS Trust who is now the clinical lead at the small Welsh company, which was spun out of Bridgend’s Princess of Wales hospital in 2005. “You do get a surprise when you take [the pouch] off on day four and see how much cleaner the wound looks.”
As larvae feed on dead tissue in a wound, they release chemicals that break down dead tissue into a liquid that they drink, according to Chelsea and Westminster hospital, which offers larval therapy. They also take up bacteria, which are destroyed within their gut, but do not eat healthy tissue. When applied to the wound the larvae are the size of an uncooked grain of rice, and grow to around 10-12mm during treatment. They cannot bite, since they do not have teeth, and they cannot multiply.
BioMonde’s Bridgend site has a suite of cleanrooms that only staff in specialized garments with hair nets, face masks and overshoes can enter. The “fly room” houses 24,000 male and female greenbottle flies, which are fed on a protein diet, in boxes covered in brown ladies’ tights to maintain the right humidity and temperature (the firm found at its sister site near Hamburg that tights worked better than a complex ventilation system). Micah Flores, an entomologist and R&D project manager, explains that male flies can be easily distinguished from females because the eyes touch on males, whereas on females there is a gap between them.
By the third or fourth week, the flies start laying eggs that are collected twice a week. The egg clumps are separated in a rotary shaker, disinfected twice, vacuum-drained and rinsed, then transferred to a stack of 10 plates which can each take 200 eggs.
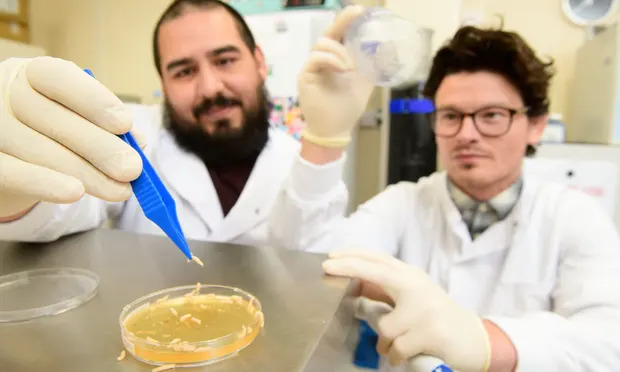
To check they are clean, a sample is poured into a microbiological broth which darkens in the presence of bacteria, explains Daniel Morris, the R&D project manager. The eggs hatch in less than a day inside 2-meter-tall incubator cabinets, and the larvae are collected and disinfected.
In the final step, Jayne Cotton, who has worked here for 22 years, picks up the larvae with a pipette and drops them into polyester pouches, which are sealed, rolled up and put into tubes. In the next room, Tina Giddings labels and packages the tubes with an information leaflet. Both have been with the business since its NHS days; all of the 30 production staff are women from the area.
–
Each order is made to prescription, on a named patient basis, and is typically delivered the next day. BioMonde supplies more than 5,000 treatments to about 250 NHS hospitals every year – a treatment often involves several pouches – and up to 15,000 in the rest of Europe.
There is undoubtedly a yuck factor in terms of the disgust felt by some patients and nurses, but Phillips says that “by the time patients are having larval therapy they are pretty open to it because they’ve tried everything”. Some may feel a tickling sensation and the larvae’s secretions emit a “musty, ammoniac smell” although some of the wounds are malodorous too, she says.
Aside from improving patients’ quality of life, maggots are also very cost effective, notes Nigam. While one pouch costs about £250, depending on the size, the speed with which maggots clean wounds saves a lot of nursing time and potentially the cost of surgical debridement (the medical removal of dead tissue) and could help avoid amputations. “Some patients have stagnant ulcers for two years and all this time they are being treated with different dressings,” she said.
Nigam and her team at Swansea University have found a small antibacterial molecule in maggots that kills MRSA and other bacteria, and are looking for funding for further research to synthesize the molecule so it can be used as a tablet against infections more widely.
Another area of research focuses on maggots’ wound-healing properties. “Clinical and anecdotal evidence suggested that maggots improve or accelerate and stimulate a wound to heal,” says Nigam. “We were really interested in why this could be possible when that’s of no evolutionary interest to the maggot at all. We’ve discovered that it’s more than likely an inadvertent happening.
“The growth factors [hormones] that are produced have a very similar structure to the human molecules and that is how perhaps by accident the human wound is stimulated to heal faster. We’re going to investigate that further.”
To help reach more squeamish patients, BioMonde is also exploring how to offer the beneficial effects of larval therapy without the presence of maggots – trying to find ways of harvesting the up to 50 enzyme secretions the grubs produce.
Work has begun on this project, and Gareth Kempson, the chief executive, says it could open up wider use in ophthalmology, to treat dry eye disease; in dentistry to treat gum and other infections; and in cosmetics, for exfoliation. “We expect to have products available within the next two years.”
–
Topics
Most viewed
- –
- –
- –
- –
- –
Most viewed