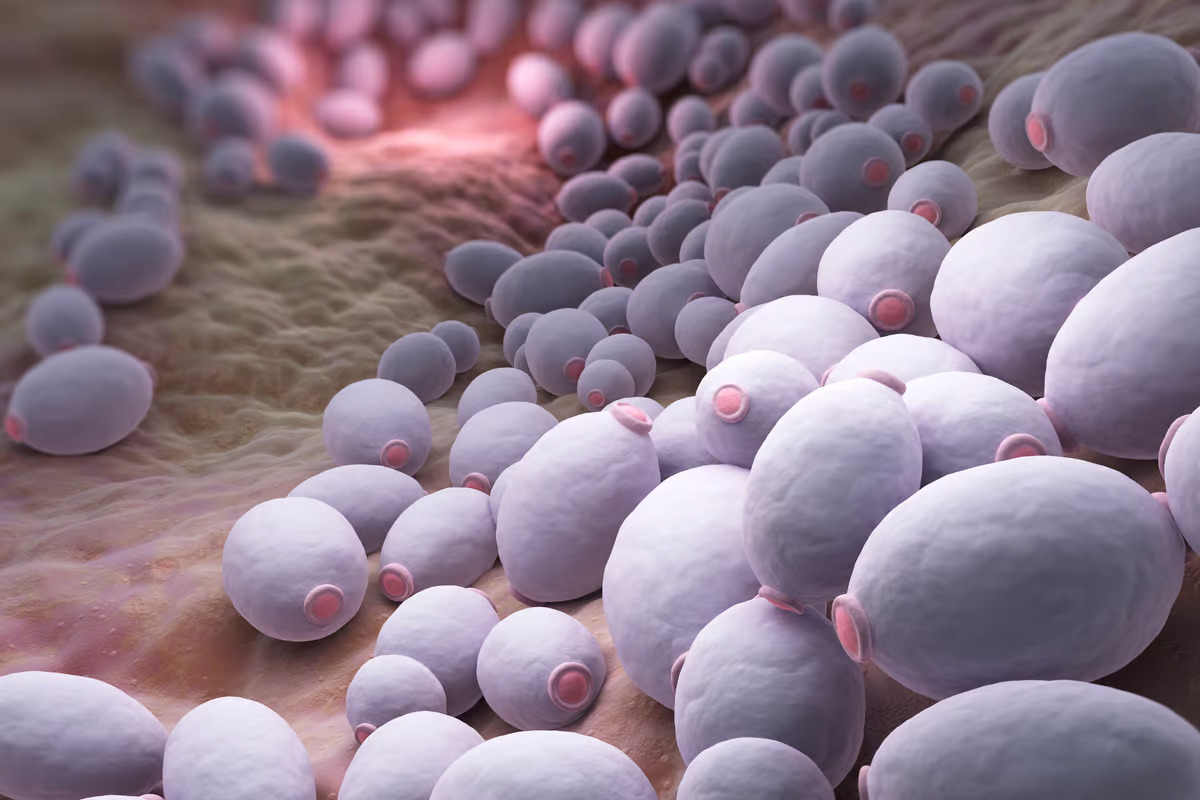
High levels of antibodies targeting Candida albicans, a common gut fungus, were linked to the most severe cases of COVID. Depositphotos
–
One hypothesis presented in 2022 suggested a person’s blood type plays a crucial role in determining the severity of COVID. But another earlier study pointed to gut bacteria differences influencing both disease severity and long COVID risk.
Hundreds of recent studies have explored the relationship between our bacterial gut microbiome and COVID but few have focused on the less popular fungal populations within us. Known as the mycobiome, it was only a decade ago that scientists discovered our guts carry a resident population of fungi. Knowing this fungal population has been associated with inflammatory changes in the body, a new study led by researchers from Weill Cornell Medicine set out to investigate whether there was a direct link between the mycobiome and severe COVID.
The first stage in the research involved studying blood samples from 91 COVID patients (25 with mild or moderate illness and 66 with severe disease). Another 36 blood samples were taken from healthy subjects. It was quickly discovered that those patients experiencing severe COVID had high volumes of immune antibodies that were tuned to target specific gut fungal populations.
Looking at fecal samples from a small subset of patients one fungus species in particular seemed to stand out in the sickest subjects, Candida albicans. The researchers could draw a distinct correlation between increasing levels of Candida and COVID disease severity.
To further home in on this compelling correlation the researchers colonized a collection of healthy mice with Candida fungus isolated from human COVID patients. The mice were then infected with SARS-CoV-2 and the researchers noted the animals experienced a significantly greater inflammatory response to the virus compared to a group without the fungus. Even more compelling, the heightened inflammatory response to SARS-CoV-2 in the mice could be tamped down by administering antifungal drugs.
Paul Griffin, an infectious disease expert from the University of Queensland, says this new research is interesting and comprehensive but not without limitations. Alongside the relatively small sample size, Griffin notes the patients included in the study were all from 2020, when the virus was circulating in a very different form and before vaccines emerged.
“Nonetheless, this study raises many possibilities including perhaps being able to look at who might be a greater risk of more severe COVID based on their mycobiota,” Griffin explained in an article for The Conversation. “There may even be a possibility of trying to change the mycobiota to reduce the risks from COVID infection. But to get to these points we need a lot more research.”
In a commentary on the new study Katherine Lagree and Peter Chen, from Cedars-Sinai Medical Center, say the findings raise lots of questions that need to be answered. It’s particularly unclear, for example, exactly how fungi in the gut can tip the body into a pro-inflammatory state when infected with SARS-CoV-2. But Lagree, Chen and Griffin indicate the study affirms our mycobiome does play a role in general health while reiterating the need for more research into the fungal inhabitants.
“These intriguing findings highlight the immunological effects of the mycobiome in viral-mediated pathology and will stimulate future investigations into how fungal dysbiosis modulates human health and disease,” conclude Lagree and Chen.
The new study was published in Nature Immunology.
–