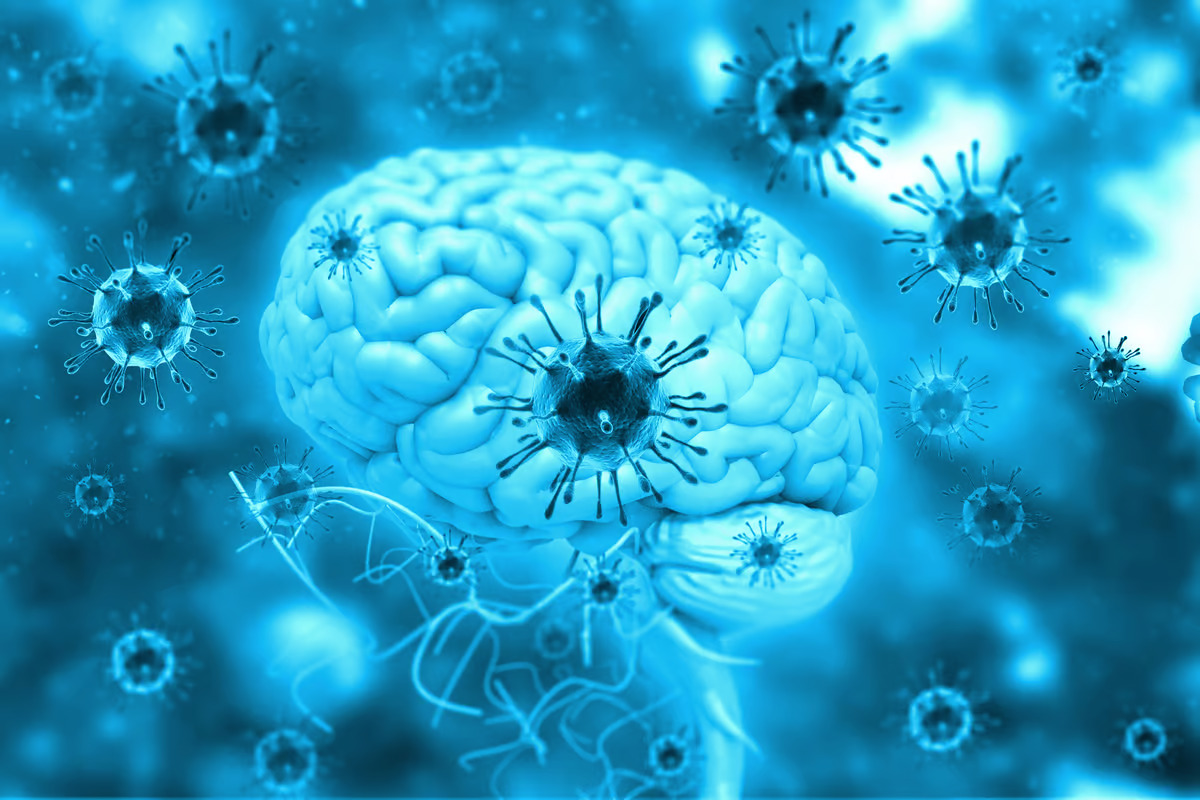
 The findings indicate inflammatory signals to the brain, via the vagus nerve, are responsible for the neurological symptoms associated with COVID. Depositphotos
The findings indicate inflammatory signals to the brain, via the vagus nerve, are responsible for the neurological symptoms associated with COVID. Depositphotos
Two hypotheses quickly emerged. One school of thought suggested these neurological issues were caused by the virus directly infiltrating the brain and infecting brain cells. Through this process, neurons were destroyed and the body’s inflammatory response then caused even more damage.
The other hypothesis argued secondary systemic inflammation was the source of these neurological symptoms. The virus was not directly damaging the brain but the body’s excessive immune response to the infection was causing the problems.
Evidence has since emerged backing both ideas. Animal and cell studies, for example, have clearly demonstrated the virus can hypothetically infect brain cells. Of course, proving this is happening in humans is nearly impossible since we can’t exactly put a living brain under the microscope. So autopsy investigations have relied mostly on looking for faint traces of SARS-CoV-2 in tissue samples. And some studies have successfully detected signs of the virus in the brain, but these findings haven’t been enough to conclude SARS-CoV-2 is actually infecting neural cells.
To date, the inflammation hypothesis has been a little more convincing. Four years into this pandemic it is clear COVID is harmful to the brain, and several studies have effectively established signs of significant inflammatory damage. But again, questions have emerged around what is triggering the inflammatory damage.
A new study, from a team of European researchers led by scientists at Charité – Universitätsmedizin Berlin, decided to tackle the mystery of COVID’s effect on the brain by starting at the very beginning. They first looked closely at brain tissue samples from 21 individuals who died from severe COVID infections.
Much like prior studies, traces of SARS-CoV-2 were found in the brain tissue samples, but most significantly the researchers could not detect any signs of direct neuron infection.
“We assume that immune cells absorbed the virus in the body and then traveled to the brain,” explained study co-author Helena Radbruch. “They’re still carrying the virus, but it doesn’t infect cells of the brain. So coronavirus has invaded other cells in the body, but not the brain itself.”
Homing in on the specific molecular effects of COVID, the researchers detected major changes to cells in the cranial nerve nucleus. These are the neurons that comprise the brainstem, running up through the neck and face, into the brain. The findings suggest localized inflammatory reactions triggered by COVID subsequently activated these communication pathways to the brain, causing the neurological symptoms we associate with the disease.
“In simplified terms, our interpretation of our data is that the vagus nerve ‘senses’ the inflammatory response in different organs of the body and reacts to it in the brainstem – without there being any actual infection of brain tissue,” said Radbruch. “Through this mechanism, the inflammation does spread from the body to the brain in a way, which can disrupt brain function.”
The narrow nature of the research makes it hard to know if these inflammatory markers account for the longer-term symptoms seen in long COVID patients. Looking at a comparative cohort of deceased patients, who died some time after their acute illness, the researchers saw many of these biomarkers return to normal. However, further work in long COVID patients will be necessary to find out whether this inflammatory cascade lingers in those few with persistent symptoms.
“We think it’s possible that if the inflammation becomes chronic, that could be what causes the neurological symptoms often observed in long COVID in some people,” added Christian Conrad, another co-author on the study. “To follow up on this suspicion, the team of researchers is now planning to study the molecular signatures in the cerebral fluid of long COVID patients in greater detail.”The study was published in the journal Nature Neuroscience.
Source: Charité – Universitätsmedizin Berlin
–