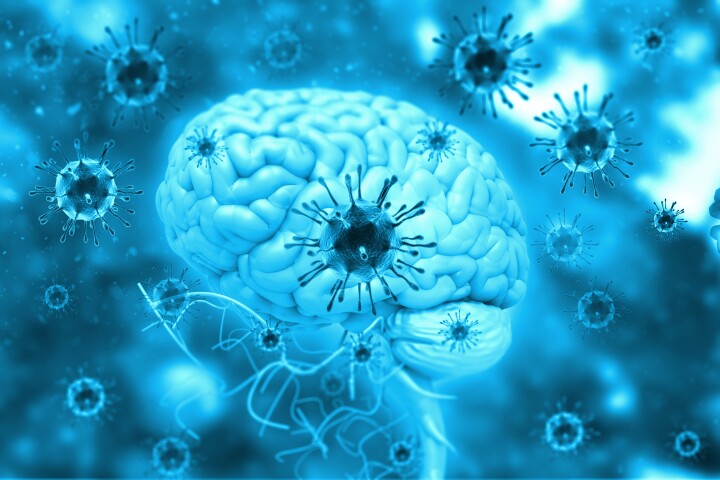
The brain and spinal cord have a limited capacity to regenerate after an injury. Following a primary injury caused by stroke, traumatic brain injury or spinal cord injury, inflammation and the formation of scar tissue cause secondary tissue damage that’s hard to heal.
Repairing a brain injury using neural stem or progenitor cells, which can self-renew and differentiate into specific brain cells like neurons and glial cells, holds great promise. However, the stem cells need to be delivered to the tissue in a medium that ensures their survival and subsequent growth.
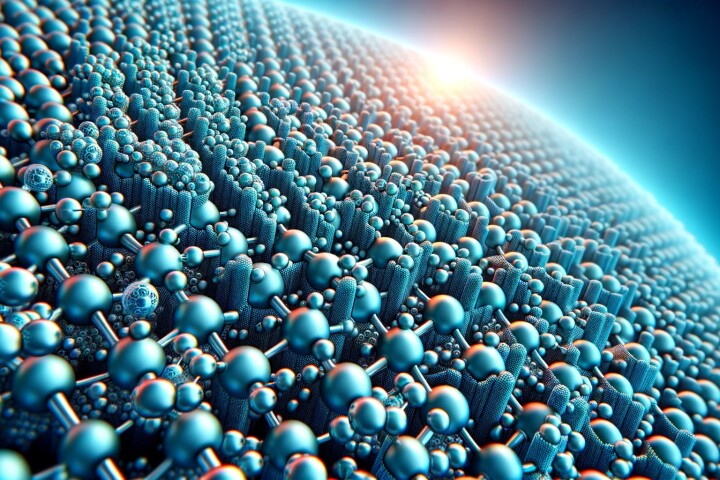
Researchers from Ruhr University Bochum and the University of Dortmund in Germany have developed a positively charged hydrogel medium that guides the differentiation of neural stem cells into particular cells that could help regenerate injured brain tissue.
“Our goal was to create an artificial environment for cells that mimics the natural cell environment in the brain,” said Kristin Glotzbach, the study’s lead author. “Cells have a negatively charged coating, also called the pericellular matrix. This means they adhere particularly well to positively charged substrates.”
Neural stem cells can differentiate into three cell types: neurons, astrocytes, and oligodendrocytes. Neurons are the fundamental brain and nervous system units, responsible for receiving sensory input from the outside world, sending motor commands to muscles, and transforming and relaying electrical signals at every step in between. Astrocytes and oligodendrocytes are subtypes of glial cells which provide support to, connect and protect neurons.
Using hydrogels as a medium for stem cells is not a new thing. But relatively few researchers have used positively charged, or cationic, hydrogels. So, for the current study, the researchers set about synthesizing one. The key was the cationic molecule trimethylaminoethyl acrylate (TMAEA); with it, they created six gels (G1 to G6) with increasing cationic charge concentrations. G1 was not charged and acted as a neutral reference gel.
Using neural stem and progenitor cells (NSPC) from embryonic mouse brains, the researchers placed 40,000 of the cells into each of the six hydrogels. They found that the gel’s cationic charge greatly influenced the cells’ differentiation. G5, the second most positively charged hydrogel, had significantly more neurons than the uncharged G1. In contrast, the lower-charged G2 and G3 hydrogels harbored significantly more astrocytes than the highly-charged G6. The highest number of oligodendrocytes was found on G1, G3 and G4 and the lowest on G6, but overall, the percentage of oligodendrocytes was significantly lower compared to neurons and astrocytes. Taken together, the cell differentiation profiles of hydrogels G1 to G6 showed that each cell type responded best to a certain cationic charge concentration.
While the NPSCs survived on the cationic hydrogels, the researchers found that adding fibroblast growth factor 2 (FGF2), which regulates many cellular functions in the body, including cell proliferation and differentiation, increased the cells’ survival and rate of division.
Being able to guide stem cells to differentiate into specific brain cells has advantages, say the researchers.
“Depending on the injury, different cell types need to be replaced,” Glotzbach said. “In certain diseases, glial cells are also attacked, which you then want to replace. For example, in multiple sclerosis, the insulation of the nerve cells, which is formed by oligodendrocytes, is destroyed.”
The researchers plan to continue fine-tuning their hydrogel, including developing a gel that can be used to fill cavities in brain tissue following injury.
“In future studies, we would like to equip the positively charged gels with peptides or components of extracellular matrix molecules and thus stimulate the natural environment of the cells even better,” said Glotzbach.
The study was published in the journal ACS Biomaterials Science & Engineering.
Source: Ruhr University Bochum
–